Case of the Month ...
Case History
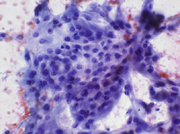
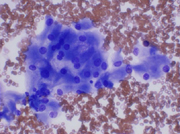
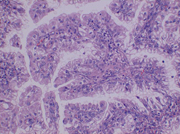
A 29-year-old female presented with a two-month history of persistent left flank pain. She was treated for a presumed urinary tract infection. A CT scan demonstrated a 2.6 cm mass in the superior pole of the left kidney. A CT-guided fine needle aspiration was performed. The Papanicalaou-stained slide revealed a cellular smear consisting of some cohesive clusters of cells with round, uniform nuclei with finely granular chromatin, and prominent nucleoli. (Figure 1) The cytoplasm was abundant and finely granular. (Figure 2) The Diff Quik-stained slide revealed mainly single cells and small clusters with the same nuclear and cytoplasmic features.(Figure 3) No psammoma bodies were seen. A few cells with large cytoplasmic vacuoles were present.
Diagnosis & Discussion
click on image for larger version
Diagnosis: Papillary Renal Cell Carcinoma
Discussion: Papillary renal carcinoma accounts for up to 15% of all renal cell carcinomas. At least half of the lesion must show well-defined papillae. They are typically composed of low-grade cells, and are thought to be less aggressive than usual renal cell carcinoma, except when significant nuclear atypia is present. Renal cell carcinomas are typically solitary but can vary greatly in size. The majority arise in the superior pole of the kidney. Renal cell carcinoma is the most common malignancy of the kidney. It is more common in men, typically around the age of fifty.
Fine needle aspiration of papillary carcinoma is typically cellular. Characteristically, there are fibrovascular stalks surrounded by a layer of tumor cells. The stalks are often distended by lipid-laden macrophages. The tumor cells are typically cuboidal to columnar, with bland nuclei and high nuclear/cytoplasmic ratios. Significant atypia is unusual in pure papillary renal cell carcinoma. The cytoplasm is scant to moderate, and clear or granular in character. Necrosis and hemorrhage may be seen. Pleomorphism, multinucleation and mitotic figures are infrequent.
It was difficult to identify true papillae in this case. Also, the abundant granular cytoplasm was very consistent with an oncocytic neoplasm. The differential diagnosis also includes papillary transitional cell carcinoma, metastatic papillary adenocarcinomas, chromophobe renal cell, and ordinary renal cell carcinoma.
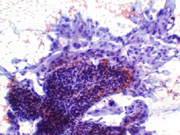
The lining of the papillae in transitional cell carcinoma tends to appear more stratified; there may be a high-grade component, as well as mucin positivity. Papillary renal cell carcinoma is less stratified, the cells have vacuolated cytoplasm, and there is a background of histiocytes and necrosis. Metastatic carcinoma is often mucin positive, which is rare in renal cell carcinoma. Ordinary renal cell carcinoma has fewer, shorter papillae, with more single cells. The cells of ordinary renal cell carcinoma are often more atypical, have more abundant cytoplasm, and consequently, have lower nuclear/cytoplasmic ratios than cells of papillary renal cell carcinoma. The diagnosis of oncocytoma requires that the tumor be composed exclusively of oncocytes. This tumor is not. Some of the cells are clear. Chromophobe renal cell carcinoma tends to have a characteristic alveolar or nesting pattern of cells, with well-defined cell borders and abundant cytoplasm. It does not form papillary structures, like we see in this case. The cytoplasm has a pale, acidophilic quality and there is often a clear perinuclear region. The nuclei are typically wrinkled, raisin-like, and hyperchromatic, unlike the round nuclei with finely granular cytoplasm seen in this case.
Grading of the tumor (ie, nuclear size and atypia) correlates well with the prognosis. As the grade increases, cellular and nuclear atypia increase, while intercellular cohesion decreases.
Unfortunately, about a quarter to a third of patients have metastases at the time of diagnosis. The presence or absence of metastases is the single most important factor in determining survival.
Surgical correlation: The patient underwent a laparoscopic partial left nephrectomy. The histology showed definite papillary structures, and the case was signed out as papillary renal cell carcinoma. (Figure 4)
This case is provided by Drs. Amanda Ashton Sager and Alaa Afify from the Department of Pathology, University of California , Davis Medical Center , Sacramento CA .