Case of the Month ...

Case History
This is a liquid based (SurePath) vaginal cuff pap test from a 45-year-old female. Her past medical history is significant for a radical hysterectomy in 1999 for a stage IB1 cervical squamous cell carcinoma, followed by radiation and chemotherapy. She subsequently developed a recurrent squamous cell carcinoma of the vaginal cuff in 2004, which was treated with radiation. Two years later she developed bilateral hydronephrosis and underwent a right nephrectomy for severe chronic pyelonephritis and multiple calculi.
Diagnosis & Discussion
click on image for larger version
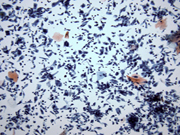
Figure 1
Cytologic Diagnosis: Numerous benign glandular cells present consistent with vesico-vaginal fistula. The glandular cells are arising from cystitis glandularis.
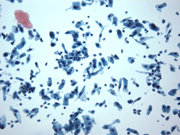
Cytologic Features: The pap test shows numerous columnar cells, with basally located bland nuclei (Figures 1-5). The nuclear to cytoplasmic ratio is low. There is no nuclear hyperchromasia. Inconspicuous nucleoli are observed. The cytoplasm is delicate, fluffy and rare vacuoles are observed, indicating glandular origin. There are no cilia or terminal bars present in any of the columnar cells. Metaplastic and atrophic squamous cells are observed in the otherwise clean background.
Discussion: The presence of benign glandular cells on a Pap smear from women after undergoing a total hysterectomy can range from 1% to 13%. The most common and well known reasons for this are: a wrong history (supra-cervical hysterectomy or no hysterectomy), vaginal adenosis, metaplasia, endometriosis, fallopian tube prolapse, primary or metastatic adenocarcinoma and fistulas. Glandular cells that cytologically don't resemble endocervical cells can be present as a result of fistulas. The patient's clinical history and correlation with radiologic findings are important in determining the exact origin of such glandular cells. In a case of vesico-vaginal fistula benign urothelial cells, umbrella cells or columnar shaped glandular cells (i.e. cystitis glandularis or other metaplastic changes of the urothelium) can be seen on Pap smears, whereas in recto-vaginal fistula columnar appearing cells are noted forming rosette-like glands or sheets with goblet cells associated with a dirty background.
n this particular patient a PET scan obtained 2 years following completion of radiation therapy showed a crescent shaped fluid collection within the vaginal cuff with absence of tracer filling in the bladder, consistent with a widely patent vesicovaginal fistula. The patient also complained of urinary leakage. We concluded that the origin of the benign glandular cells on this Pap test are from the urinary bladder. The abundance of columnar cells in this case are most likely arising from cystitis glandularis, a benign metaplastic change observed in the urinary bladder. These cells are distributed singly, rather than in a honeycomb or picket fence arrangement, which would be more characteristic of endocervical cells. In view of the patient's clinical history of having undergone a total hysterectomy, it would be unusual to encounter a vaginal cuff smear with a predominance of endocervical cells.
References:
- Richard M. DeMay: The Pap Test, ASCP Press, 2005; 188-190.
- Eren F, Savci D, Erbraut I, Gokaslan H.: Benign glandular cells in posthysterectomy vaginal smears: the incidence is higher than expected. Cytopathology 2004 Aug; 15(4): 195-9.
- Tambouret R, Pitman MB , Bell DA.: Benign glandular cells in posthysterectomy vaginal smears. Acta Cytol. 1998 Nov-Dec; 42(6): 1403-8.
- Ponder TB, Easley KO, Davila RM. : Glandular cells in vaginal smears from posthysterectomy patients. Acta Cytol. 1997 Nov-Dec; 41(6):1701-4.
- Bewtra C.: Columnar cells in posthysteretcomy vaginal smears. Diagn. Cytopathol. 1992;8(4): 342-5.
- Ramirez NC , Sastry LK, Pishadori LP.: Benign glandular and squamous metaplastic-like cells seen in vaginal Pap smears of posthysterectomy patients: incidence and patient profile. Eur.J.Gynaecol. Oncol, 2000; 21(1):43-8.
Acknowledgement: Krisztina Z. Hanley M.D., and Talaat S. Tadros M.D.
Emory University Hospital and Grady Memorial Hospital , Atlanta , GA