Case of the Month ...
Case History
A 34-year old Hispanic man presented for the evaluation of new-onset seizures. During the patient’s neurological workup, a CT of the abdomen found a 1.7 x 1.1 cm well circumscribed lesion within the pancreatic tail. A fine needle aspiration of the mass in the tail of the pancreas was performed.
Diagnosis & Discussion
click on image for larger version
Figure 1
Image Figures:
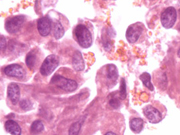
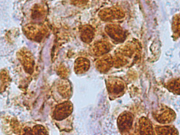
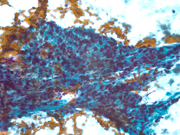
- Figure 1: FNA cytology smear of pancreas, Papnicolaou stain, X 400
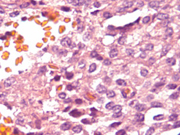
- Figure 2: FNA cytology smear of pancreas, Papanicolaou stain, X 600
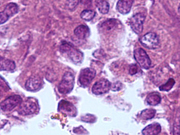
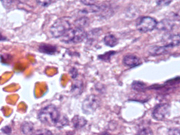
- Figure 3: FNA cell block, H&E, X 400
- Figure 4: FNA cell block, H&E, X 400
- Figure 5: FNA cell block, H&E, X 600
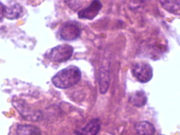
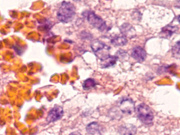
- Figure 6: FNA cell block, Vimentin Immunoperoxidase stain, X 400
- Figure 7: FNA cell block, Beta-catenin Immunoperoxidase stain, X 400
- Figure 8: Surgical resection of pancreas, H&E, X 200
- Figure 9: Surgical resection of pancreas, H&E, X 400
- Figure 10: Surgical resection of pancreas, H&E, X 600
Diagnosis: Solid Psudopapillary Tumor of the Pancreas
(Also known as: Papillary epithelial neoplasm, papillary-cystic neoplasm, solid and papillary epithelial neoplasm, papillary and solid neoplasm, and solid and cystic tumor).Cytologic Findings:
- Cellular specimen
- Branching fibrovascular structures
- Bland, uniform cells with benign nuclear features
- Round to oval eccentrically located nuclei
- Nuclear grooves
- Indistinct cell borders
- May see large, clear cytoplasmic vacuolation (on Diff-Quick stained smears)
- Background of blood, macrophages, and necrotic debris
Discussion: Solid-Psuedopapillary Tumor (SPT) is a rare tumor (1-2% pancreatic tumors) of the pancreas that occurs predominantly in young female patients within the second and third decades. This tumor is rarely seen in the elderly or in men. Patients usually present with a large asymptomatic abdominal mass which is often found incidentally within the body or tail of the pancreas. SPTs are usually solitary but can be multifocal, and range from eight to ten centimeters in size. Grossly, SPTs are both solid and cystic possessing areas of hemorrhage and necrosis. The cystic spaces that form in SPTs are not true cysts but are the effect of necrosis and degeneration due to ischemia. Microscopically, peudopapillary architecture, hyaline globules, clusters of uniform cells, and grooved nuclei may be seen
The differential diagnosis of SPTs is vast and includes:
- Pancreatic pseudocyst
- Cystic neoplasms
- Mucinous cystic neoplasm- Found in the body/tail of pancreas; but is seen in an older population of women (40-50 years of age). Mucin containing epithelium will be present.
- Serous cystadenoma- Found in the body/tail of the pancreas of elderly women. Will see cytoplasmic glycogen and no mucin.
- Partially cystic ductal adenocarcinoma
- Partially cystic acinar cell carcinoma- CK (+), vimentin (-), Neuron Specific Enolase (NSE) (-), Amylase/Lipase/Trypsin (+), and pancreatic hormones (-).
- Pancreatic endocrine neoplasm- Will have a nested architectural pattern. CK (+), Vimentin (-), NSE (+), Amylase/Lipase/Trypsin (-), pancreatic hormones (+).
- Pancreatoblastoma – Seen in children. Will have squamoid corpuscles
The diagnosis of SPT is made based on the clinical presentation, location of tumor, histological findings, and immunohistochemical staining. SPTs express positive immunohistochemical staining for vimentin, CD56, alpha-1-antitrypsin and neuron-specific enolase. Epithelial markers (keratins) may be focal or weakly positive. Synaptophysin is commonly positive in SPTs; however, chromogranin is usually negative. Immunohistochemical staining for Amylase/Lipase/Trypsin are negative, as well as those for pancreatic hormones. There may be positive immunohistochemical staining for CD10, Beta- catenin, CD117 (c-kit), Progesterone receptor, and the beta form of estrogen receptor.
SPTs are considered to be tumors of low malignant potential and more than 80% of SPTs are cured by surgical resection. However, metastases may be seen in a small percentage of patients. When metastasis occurs, it is usually to the liver or peritoneum.
Patient follow-up: The patient underwent a brain biopsy. Histologic examination found non-caseating granulomata and a diagnosis of neurosarcoidosis was rendered. Subsequent distal pancreatectomy was performed. A 1.5 x 1.5 cm circumscribed, focally hemorrhagic tumor within the tail of the pancreas was identified and the diagnosis of SPT was rendered (Vimentin- positive, Progesterone Receptor- positive, alph-1-antitrypsin- positive, and Neuron specific enolase- positive).
References:
- Atkinson, B.F. Atlas of Diagnostic Cytopathology. 2 nd Edition. Saunders, Philadelphia, 2002; 562, 574.
- Adsay, NV. Cystic lesions of the pancreas. Modern Pathology. 2007; 20:S71-S93.
- Bostwick, D.G. and Liang, C. Essentials of Anatomic Pathology. 2 nd Edition. Humana Press, New Jersey, 2006; 1363-1364.
- Cibas, E.S. and Ducatman, B.S. Cytology: Diagnostic Principles and Clinical Correlates. 2 nd Edition. Saunders, New York, 2003; pp. 375-376.
- Demay, RM. Practical Principles of Cytopathology. 1 st Edition. ASCP Press, Chicago, 1999; 332.
- Jhala, N, Siegal G.P., and Jhala, D. Large, Clear Cytoplasmic Vacuolation: An Under-recognized Cytologic Clue to Distinguish Solid Pseudopapillary Neoplasms of the Pancreas From Pancreatic Endocrine Neoplasms on Fine-Needle Aspiration. Cancer Cytopathology. 2008 (114) 4: 249-254.
- Rosai, J. Rosai and Ackerman’s Surgical Pathology. 9 th Edition. Mosby, New York, 2004; 1082-1083.
Acknowledgment: Submitted by Sharenda L. Williams, M.D. and Talaat S. Tadros, M.D., Emory University Hospital and Grady Memorial Hospital, Atlanta, GA.