Case of the Month ...
Case History
A 51 year-old man with a history of lung carcinoma, status post right upper lobectomy, was found to have elevated creatinin and blood urea nitrogen levels on a routine exam. A 2.7 cm hypoechoic solid mass in the mid pole of the left kidney was present on ultrasound examination. An ultrasound-guided fine needle aspiration biopsy of the mass was performed. See figures.
Diagnosis & Discussion
click on image for larger version
Figure 1
Image Figures:
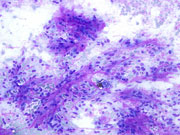
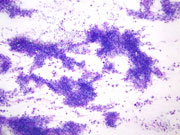
- Figure 1: FNA cytology smear of kidney, Diff-Quik stain, × 100
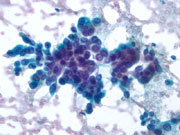
- Figure 2: FNA cytology smear of kidney, Diff-Quik stain, × 200
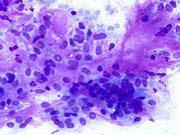
- Figure 3: FNA cytology smear of kidney, Papanicolaou stain, × 200
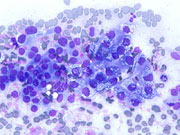
- Figure 4: FNA cytology smear of kidney, Papanicolaou stain, × 400
- Figure 5: FNA cytology smear of kidney, Diff-Quik stain, × 400
- Figure 6: FNA cytology smear of kidney, Diff-Quik stain, × 400
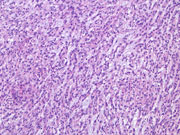
- Figure 7: Surgical resection of kidney, H&E stain, × 100
- Figure 8: Surgical resection of kidney, H&E stain, × 200
Questions:
- What is the diagnosis?
- Sarcomatoid renal cell carcinoma
- Renal mucinous tubular and spindle cell carcinoma
- Angiomyolipoma
- Papillary renal cell carcinoma
- What cytomorphologic features are characteristic for this entity?
- True papillary clusters of epithelial cells and no myxoid/mucinous matrix
- True papillary clusters of epithelial cells and myxoid/mucinous matrix
- Branching clusters of epithelial cells and no myxoid/mucinous matrix
- Branching clusters of epithelial cells and myxoid/mucinous matrix
- Which of the following immunophenotypic features is consistently seen in this entity?
- Positive vimentin and positive alpha-methyl CoA racemase
- Negative vimentin and positive CD10
- Neagtive EMA and positive CD10
- Negative CK7 and positive CK20
- This tumor is most likely arising from?
- Proximal convoluted tubules
- Bowman's capsule
- Henle's loop and collecting ducts
- Granular cells of the juxtaglomerular apparatus
Discussion: Mucinous tubular and spindle cell carcinoma (MTSCC) of the kidney is a rare, recently recognized, low grade renal cell tumor. Initially described as “low grade collecting duct carcinoma” by MacLennan et al.,1 this tumor has been included in the World Health Organization 2004 classification as a distinct entity.2 The neoplasm is thought to originate in the distal nephron, especially Henle loop or collecting duct.3,4 Proper diagnosis and classification are important because of favorable clinical outcome in the majority of cases. The tumor shows female predominance. Histologically the neoplasm is characterized by a circumscribed lesion with interconnecting tubular and spindled architecture, low grade nuclear grade and mucinous/myxoid stroma.1-4. The cytomorphologic features of MTSCC include a cellular aspirate consisting of clusters of epithelial cells with broad trabecular and branching arrangement.5-7 The clusters can form pseudopapillary aggregates, but no true papillae are seen. Abundant metachromatic mucinous/myxoid material is seen in the background or intermixed with tumor cell clusters. The neoplastic cells have relatively bland morphology and are spindled or oval in shape. They have indistinct borders, smooth nuclear contours, and conspicuous nucleoli. Fine cytoplasmic vacuoles are present in some tumor cells. 6,7
MTSCC should be differentiated from other renal neoplasms. When spindle cells are the predominant feature, 6,7 sarcomatoid renal cell carcinoma and angiomyolipoma enter the differential. The neopalstic cells in sarcomatoid carcinoma are large with hyperchromatic nuclei and prominent nucleoli. Angiomyolipoma contains small to large amount of adipose tissue, spindled and epithelioid stromal cells which have fine evenly distributed chromatin and inconspicuous nucleoli. Papillary renal cell carcinoma may show areas of spindled cells, which can mimic MTSCC. However, the tumor cells in papillary renal cell carcinoma form true papillary structures and have finely granular cytoplasm. Psammoma bodies and macrophages may be visible in the background. In cases with more prominent oval or epithelioid cell morphology, 5 clear cell (conventional) and papillary renal cell carcinoma should be considered as well as collecting duct carcinoma. The neoplastic cells in these tumors show more prominent cytological atypia compared to the bland cytomorphology seen in MTSCC. None of these entities demonstrate abundant metachromatic matrix, however clear cell renal cell carcinoma might contain a small amount of metachromatic basal membrane-like material.
TSCC commonly is positive for vimentin, EMA, and alpha-methyl CoA racemase. 2,3,8,9 The tumor cells are often positive for CK7 and negative for CK20. The staining for high molecular weight keratin and CK19 seem to be inconsistent. CD10 may be positive. The expression of E-cadherin is diffuse and the Ki-67 labeling index is low.10
References:
MacLennan GT, Farrow GM, Bostwick DG. Low-grade collecting duct carcinoma of possible collecting duct origin. Urology 1997;50:679-684.
Srigley JR. Mucinous tubular and spindle cell carcinoma. In: Eble JN, Sauter G, Epstein JI, Sesterhenn IA, editors. Pathology and genetics of tumors of the urinary system and male genital organs. World Health Organization Classification of Tumors, Lyo: IARC Press; 2004. p.40.
Parwani AV, Hussain AN, Epstein JI, Beckwith JB, Argani P. Low-grade myxoid renal epithelial neoplasm with distal nephron differentiation. Hum Pathol 2001;32:506-512.
Srigley J, Kapusta L, Reuter V, et al. Phenotypic, molecular and ultastructural studies of a novel low grade renal epithelial neoplasm possibly related to the loop of Henle. Mod Pathol 2002;15:182A.
Sun W, McGregor DK, Ordonez NG, Ayala AG, Caraway NP. Fine needle aspiration cytology of a low grade myxoid renal epithelial neoplasm: a case report. Acta Cytol 2005;49:525-529.
Owens CL, Argani P, Ali SZ. Mucinous tubular and spindle cell carcinoma of the kidney: cytopathologic findings. Diagn Cytopathol 2007;35:593-596.
Marks-Jones DA, Zynger DL, Parwani AV, Cai G. Fine needle aspiration biopsy of renal mucinous tubular and spindle cell carcinoma: Report of two cases. Diagn Cytopathol 2009 [Epub ahead of print].
Paner GP, Srigley JR, Radhakrishan A, et al. Immunohistochemical analysis of mucinous tubular and spindle cell carcinoma and papillary renal cell carcinoma of the kidney: significant immunophenotypic overlap warrants diagnostic caution. Am J Surg Pathol 2006;30:13-19.
Ferlicot S, Allory Y, Comperat E, et al. Mucinous tubular and spindle cell carcinoma: a report of 15 cases and review of literature. Virchow Arch 2005;447:978-983.
Otani M, Shimizu T, Serizawa H, Ebinara Y, Nagashima Y. Low grade renal cell carcinoma arising from the lower nephron: A case report with immunohistochemical, histochemical and ultrastructural studies. Pathol Int 2001;51:954-960.
Answers to the questions:
- b
- d
- a
- c
Contributed by Drs. Alexander Finkelstein and Guoping Cai, Department of Pathology, Yale University School of Medicine